 THE Western Trust is the first Health and Social Care Trust in the North of Ireland to be recognised by the Perinatal Institute for their work in preventing stillbirths.
THE Western Trust is the first Health and Social Care Trust in the North of Ireland to be recognised by the Perinatal Institute for their work in preventing stillbirths.
The Western Trust, which has maternity units at Altnagelvin Hospital in Derry and the South West Acute Hospital in Enniskillen along with the Women’s Centre at Omagh Hospital and Primary Care Complex, has been named one of the top ten in the UK for their work in preventing stillbirths by detecting small (gestational age) babies.
This work has led to a 23 per cent reduction in stillbirths in the UK compared to the previous ten-year average.
The ‘Ten Best’ units in the UK represent a three-fold increase from 18%.
The average UK detection rate is 42% compared to the Western Trust who is averaging 53%.
Now 83% of Trusts (124 Units) in the UK are using the Gestation Related Optimal Weight software (GROW) protocols, the Western Trust places in the top 10 for its detection rates and is the first HSC Trust in Northern Ireland to do so.
This is a result of the programme being fully implemented at the Trust for at least three years and demonstrates the Trust’s ongoing commitment to quality improvement since the initiative started in 2006.
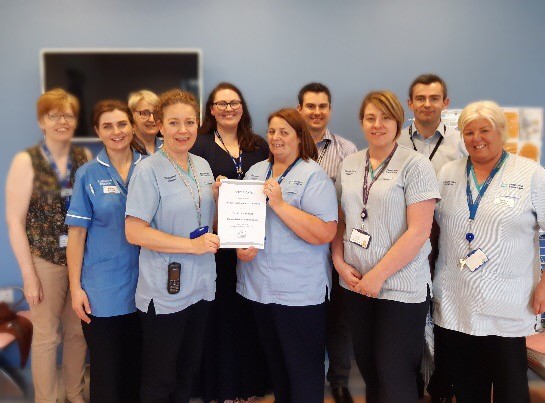
Deirdre Gill, Clinical Risk Midwife and Growth Assessment Protocol (GAP) lead for the Western Trust said:
“The midwifery and medical teams have worked together really hard over several years to make the GAP initiative work and in turn make a difference to women and their families.
“The key motivator for them has been the awareness that some adverse pregnancy outcomes maybe avoidable and this is a great example of the team putting their efforts into improving outcomes for mothers and babies.
“This is a fantastic achievement and we are extremely proud of everyone involved in this initiative.”
Deirdre added: “Previously women would have a scan and the baby’s size would be calculated on the basis of the size of the abdomen around the baby.
 “Now the mother’s BMI, ethnicity and age are taken at the booking-in appointment with her midwife and fundal height measurements are taken throughout her antenatal visits if she is low risk.
“Now the mother’s BMI, ethnicity and age are taken at the booking-in appointment with her midwife and fundal height measurements are taken throughout her antenatal visits if she is low risk.
“However, if the measurements cause concern they are sent for a scan and further investigation.
“Mothers with high-risk pregnancies now attend serial ultrasound scans to calculate the baby’s birth weight, increasing the opportunity to detect anything out of the normal.
“Risk factors include smoking, higher BMIs, diabetes and increased maternal age. Midwives who are specially trained carry out growth scans at the Trust’s Maternal and Fetal Assessment Units. This initiative is soon to be expanded to the Antenatal Clinics.”
The GAP programme, with its face to face training, e-learning modules, audit tools and other initiatives all succeed through the maternity units’ continued emphasis on robust training of in-house and front line staff.
Pathways to introduce specialised midwives to carry out Growth Scans at Consultants Clinics have been agreed.
With the help and support of Consultants, Maternal and Fetal Assessment Unit, and midwifery staff, the Trust are planning to introduce a Midwife Led Ultrasound Clinic.
Where a woman is deemed to be low risk, she will have fundal height measurements plotted on the chart by the midwife throughout her ante-natal care to monitor the growth of the baby.
The expectation is that, once plotted, they will follow a continuous curve.
 However, if there is any deviation from the curve, they will be referred into the Midwife Led Ultrasound Clinic/Women’s Ultrasound for a scan to assess baby’s growth and wellbeing, increasing the opportunity to detect any issues.
However, if there is any deviation from the curve, they will be referred into the Midwife Led Ultrasound Clinic/Women’s Ultrasound for a scan to assess baby’s growth and wellbeing, increasing the opportunity to detect any issues.
The Trust is also using The GAP SCORE audit tool to monitor missed cases of small babies which will then help initiating further changes to improve the detection rates.
Tags:




